DBT A Framework for Emotional Stability and Adaptive Response
DBT gives you concrete skills to steady your nervous system, set boundaries, and build a life that actually works
DBT helps you understand your emotional patterns and gives you the skills to respond to them with more stability and control. DBT builds four foundational skill domains - mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness - each targeting a different part of the cognitive–emotional system. Together, they train you to stay present without getting swept away, to endure emotional surges without escalating the situation, to reduce reactivity and return to baseline more quickly, and to communicate needs or boundaries with clarity and mutual respect. Over time, crises shorten, recoveries accelerate, and your internal system becomes more stable and adaptive.
DBT A Structured Approach to Stability
DBT is used to address a range of high-intensity conditions, including ADHD-related emotional dysregulation, chronic self-harm impulses, and recurring suicidal ideation. It is also effective for individuals struggling with intense mood swings, persistent relationship conflict, communication breakdowns, and patterns of impulsive behavior such as overspending, substance use, or bingeing. Treatment further supports those navigating depressive emptiness, PTSD, and complex trauma.
Clinical Targets of DBT
DBT Specialists
Scotty French, LP-MHC
Scotty is currently completing their PhD in Mental Health Counseling, bringing cutting-edge research and advanced training into sessions. As a DBT-focused clinician, they combine academic expertise with practical, compassionate care. Clients often describe their approach as both highly supportive and deeply insightful, blending the rigor of a doctoral-level perspective with the warmth of genuine human connection.
Nathaniel Terpening, LP-MHC
With over 14 years of clinical experience, Nathaniel brings a wealth of knowledge to his work. He is trained in both DBT and EMDR, allowing him to integrate skills-based strategies with trauma processing when appropriate. Clients value his calm, steady presence and his ability to guide them through both crisis moments and long-term growth.
Testimonials
“Therapy with Scotty never feels clinical or cold. They’re down-to-earth, approachable, and create an atmosphere where I actually want to open up.”
“Nathaniel has a gift for crisis intervention. In one of my darkest moments, he provided immediate support and tools to stabilize my emotions. His approach is compassionate yet effective. I'm so grateful!”
Reviews can be verified on Google and ZocDoc pages.
DBT Treatment
Treatment Grounded in Research
DBT is one of the most researched therapies for chronic emotion dysregulation, self-harm urges, and relationship instability. It combines acceptance and change strategies that have shown strong outcomes in multiple clinical trials for reducing suicidal behaviors, hospitalizations, and overall symptom severity.
Team Collaboration
At A.J.B. Counseling & Psychotherapy, DBT is delivered by clinicians trained in DBT skills and protocols, with ongoing supervision and consultation. We follow structured plans while tailoring strategies to your goals, culture, and daily realities.
Innovation
We integrate DBT with complementary methods when helpful, including trauma-informed care, EMDR coordination for trauma memories, and mindfulness-based tools. The aim is practicality: skills you’ll actually use in real life, not just in session.
Rapid and Lasting Improvement
Clients often notice earlier wins like fewer blowups, faster cooldowns, and more effective boundary setting. With consistent practice, DBT skills become automatic, so relief lasts beyond the therapy hour.
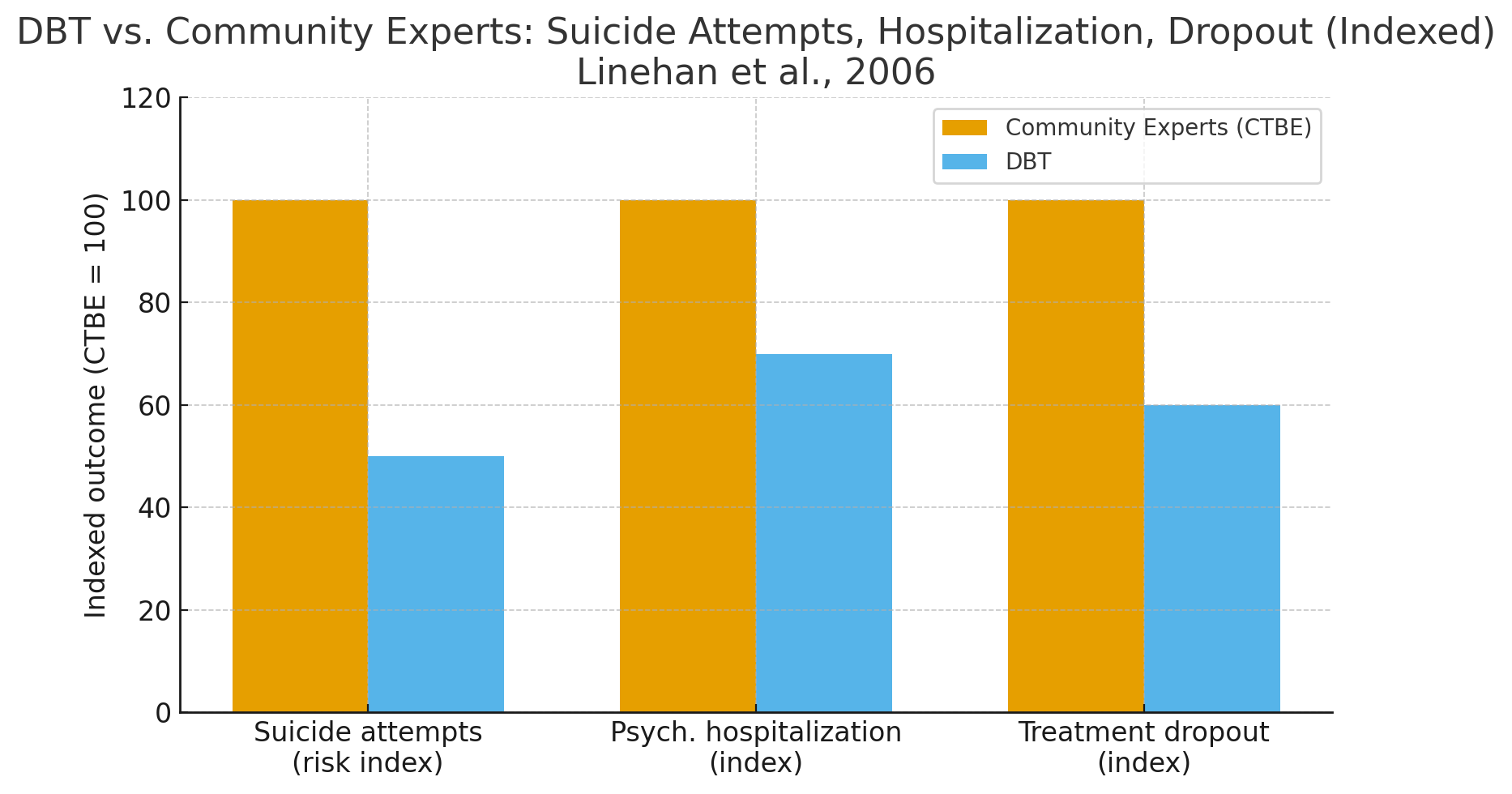
Figure 1 shows that DBT significantly reduced suicide attempts and psychiatric hospitalizations compared to treatment by community experts. After two years, DBT patients had 50% fewer suicide attempts and fewer psychiatric hospitalizations, while also maintaining higher treatment retention. Unlike many therapies where dropout is common, DBT’s structured approach kept participants engaged and safe over time.
Reference:
Linehan, M. M., Comtois, K. A., Murray, A. M., Brown, M. Z., Gallop, R. J., Heard, H. L., … Lindenboim, N. (2006). Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry, 63(7), 757–766. https://doi.org/10.1001/archpsyc.63.7.757
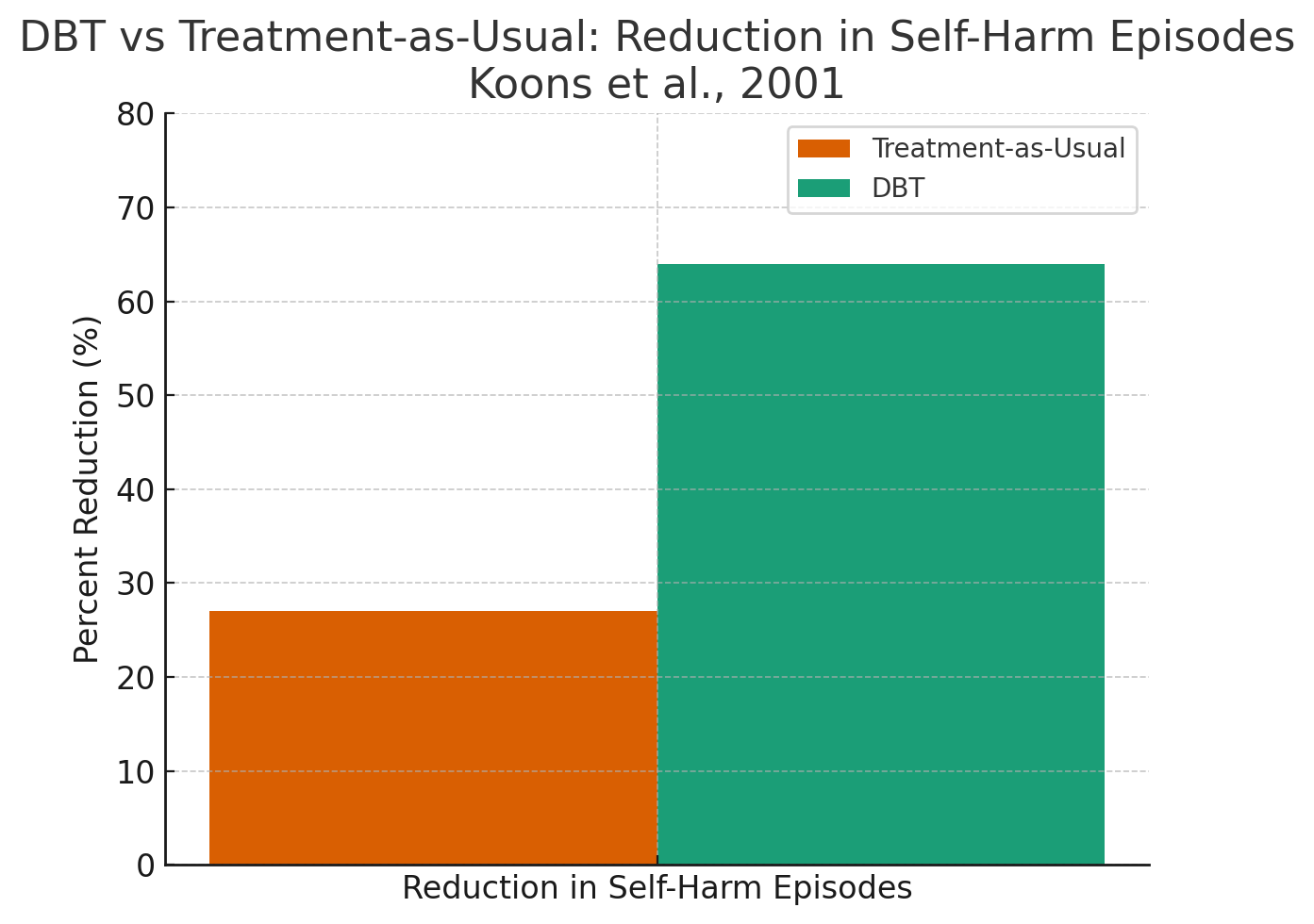
Figure 2 shows that DBT delivered greater reductions in self-harm, anger, and depression compared with treatment-as-usual in a Veterans Administration hospital trial. DBT participants experienced a 64% reduction in self-harm episodes, compared to only 27% in treatment-as-usual. In addition, DBT clients reported lower anger and depression scores and demonstrated higher treatment completion rates, showing DBT’s efficiency and durability across multiple domains of functioning.
Reference:
Koons, C. R., Robins, C. J., Tweed, J. L., Lynch, T. R., Gonzalez, A. M., Morse, J. Q., … Bastian, L. A. (2001). Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behavior Therapy, 32(2), 371–390. https://doi.org/10.1016/S0005-7894(01)80009-5
FAQs
Is DBT only for Borderline Personality Disorder?
No. While DBT is a gold-standard treatment for chronic emotion dysregulation and suicidal behaviors, it’s also effective for anxiety, depression, relationship conflict, OCD adjunct support, and trauma-related reactivity.
What if I’m in crisis?
We create a clear crisis plan early. Brief between-session coaching may be available for skill reminders when you’re stuck.
How long does DBT take?
Many clients notice meaningful improvements within the first 6 to 12 weeks. Duration depends on goals, history, and practice between sessions.
Take the First Step Toward Feeling Better
DBT helps you steady intense emotions, reduce crises, and rebuild relationships with skill and confidence.